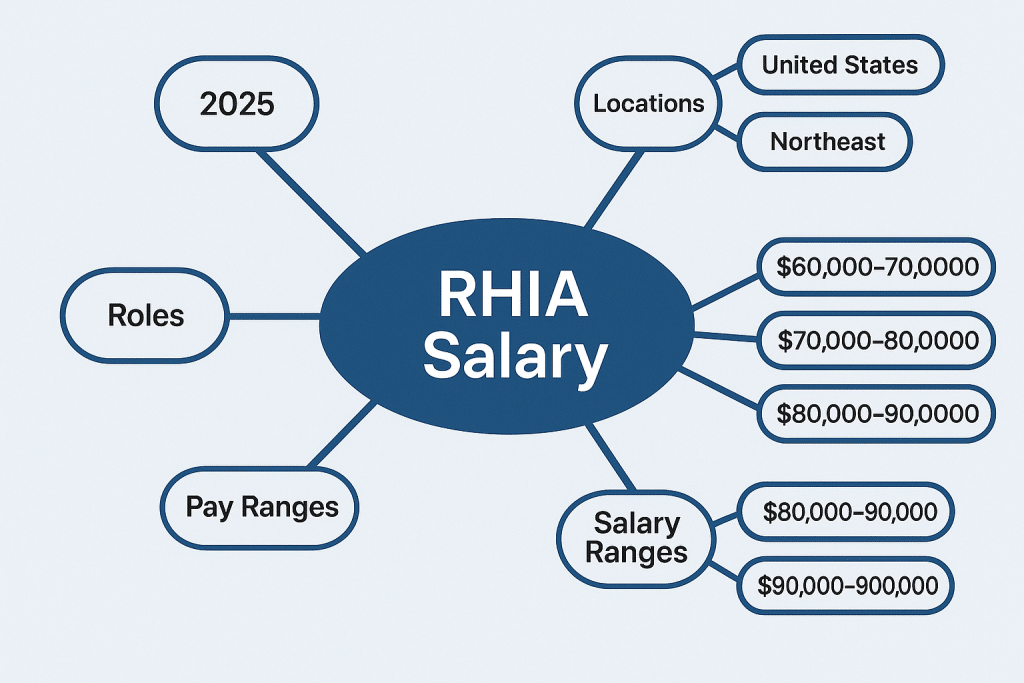
When people talk about careers in health information management, the Registered Health Information Administrator (RHIA) role usually stands out as one of the most respected and rewarding options. But after understanding what the job involves, the next thought is often, “What’s the RHIA salary like in 2025?”
The truth is, RHIA salaries can look very different depending on experience, the kind of organization, and even the state someone works in. In certain regions, RHIA managers are bringing home six figures, while in others the pay is closer to the national average. With the healthcare industry’s growing need for skilled information administrators, these numbers are continuing to shift year by year.
What This Guide Breaks Down?
| Topic | What you’ll get | Why it matters |
| Rhia Salary ranges (2025) | Realistic bands for early, mid, senior, and leadership roles, plus how org size and specialty shift pay. | Sets your baseline so you don’t under-ask or over-aim. |
| Hourly conversion | Quick math to turn annual RHIA salary into an hourly rate, with example breakouts. | Helps compare offers, shift differentials, and overtime policies. |
| State + metro hotspots | Tiered view by state and the metros that routinely pay above the average. | Targets your search to high-value markets (and balanced cost of living). |
| Roles and settings | How titles (HIM Analyst → Director) and environments (IDNs, payers, vendors) move compensation. | Shows where RHIA skills pay a premium—governance, privacy, analytics, CDI/coding operations. |
| 6–12 month pay lifts | Concrete steps: expand scope, add targeted credentials (CHPS/CDIP/CHDA), sharpen interoperability and data quality. | Builds a clear, short runway to the next salary band. |
| Helpful links (AHIMA + prep) | Official credential info, ethical study resources, and role/title guides. | Keeps you aligned with recognized standards and marketable skill |
Quick take (TL;DR)
- National snapshot (2025):
- Typical range: $65,000–$105,000
- Common midpoint: $80,000–$90,000
- Entry-level RHIA: ~$55,000–$70,000
- Leadership (Manager/Director): ~$95,000–$140,000+
- Note: Total comp can lift 5–15% with bonuses, differentials, and retirement match.
- RHIA salary per hour (fast math):
| Annual Base | Approx. Hourly (÷ 2080) |
| $70,000 | ≈ $33.50/hr |
| $85,000 | ≈ $40.85/hr |
| $110,000 | ≈ $52.90/h |
RHIA at a Glance
The Registered Health Information Administrator (RHIA) is a flagship credential for health information leaders. It shows that a professional can run HIM operations, govern data, ensure privacy and compliance, and support analytics at the enterprise level. For those looking for scope and leadership opportunities in health information management, RHIA is the path to consider.
The RHIA exam is offered by AHIMA, a leading organization in health information management that sets industry standards worldwide.
What RHIA Means
- A bachelor’s-level, CAHIIM-accredited degree plus passing the AHIMA RHIA exam
- The ability to manage the entire lifecycle of health data: capture, quality, protection, access, and use
- A skillset that blends clinical knowledge with technical expertise, along with comfort in policy, workflows, and metrics
Where RHIAs Work
RHIA professionals are in demand across a wide range of healthcare settings, including:
- Hospital and health system HIM departments
- Integrated delivery networks (IDNs) and academic medical centers
- Payers, consulting firms, and health technology vendors
- Public health agencies, government institutions, and research organizations
Key Responsibilities
RHIAs typically oversee:
- Data governance and quality management
- Health information management (HIM) operations and release of information
- Privacy and security compliance (HIPAA/HITECH, state regulations), risk management, and audit readiness
- Compliance workflows, documentation standards, and regulatory reporting
- Analytics enablement, EHR optimization, and interoperability initiatives (HL7 v2, FHIR, CCD/C-CDA)
Why RHIA Salaries Keep Rising
Several trends are driving steady salary growth for RHIA professionals:
Larger, multi-entity systems demand enterprise-level coordination and measurable outcomes
Healthcare systems require strong data governance to support value-based care and AI readiness
Regulatory complexity continues to expand (privacy, information blocking, security frameworks)
EHR optimization and interoperability projects remain ongoing and high-impact
RHIA Work
| Domain | Day-to-day examples | Salary signal (why it pays) |
| Data governance & quality | Standards, metadata, stewardship councils; data dictionaries; KPI definitions; master data clean-up | Enterprise scope, fewer rework loops, audit-ready data → higher bands |
| HIM operations | ROI workflows; chart completion/deficiencies; scanning/indexing; provider education; policy upkeep | Better turnaround and accuracy; measurable throughput wins raise comp |
| Privacy & security oversight | HIPAA risk assessments; incident response; BAAs; role-based access; OCR and internal audits | Reduced risk and penalties; CHPS/HITRUST literacy often bumps pay |
| Compliance & reporting | CMS/Joint Commission readiness; info blocking policy; release logs; statutory retention schedules | Multi-site compliance and survey success = leadership confidence (and dollars) |
| Analytics & interoperability | EHR optimization; HL7/FHIR coordination; data abstraction; BI dashboard adoption; SQL/quality checks | Cross-functional impact with IT/clinical/revenue; analytics fluency commands premiums |
Credentials at a Glance (How RHIA fits)
| Credential | Core scope | Typical pay effect |
| RHIA | Enterprise HIM leadership, governance, privacy/compliance, analytics enablement | Sets the main range in this guide; leadership lifts into six figures |
| RHIT | Technical HIM operations and data integrity | Often below RHIA; bridges to RHIA with experience/education |
| CHPS / CDIP / CHDA | Privacy-security (CHPS), documentation improvement (CDIP), analytics (CHDA) | Stacked with RHIA, these concentrate value and nudge pay up |
- Entry and maintenance:
- Bachelor’s from a CAHIIM-accredited program or AHIMA-approved pathway, then pass the RHIA exam
- Maintain CEUs and ethics standards; keep policies and tech knowledge fresh
- Good fit if you enjoy:
- Translating regulations into clean workflows
- Fixing data at the source and proving it with metrics
- Partnering with clinicians, IT, compliance, and revenue cycle to move outcomes
Tip: If “enterprise” shows up in the job scope (multi-hospital, payer, or vendor platform), your RHIA salary ceiling usually rises with it.
National Rhia Salary Ranges for 2025
Here’s how 2025 RHIA pay shakes out across stage, size, and focus. Clean ranges first, then what nudges you up a band.
RHIA salary by career stage (2025)
| Career stage | Typical titles | Base range | Common midpoint | To reach top band |
| Early career (0–2 yrs + RHIA) | HIM Analyst, ROI Specialist, Privacy/Compliance Assistant | $55,000–$70,000 | ~$62,000–$66,000 | Internship + practicum impact, early KPI ownership, SQL/BI basics |
| Mid-career (3–6 yrs) | RHIA Generalist, Privacy/Compliance Analyst, Data Governance Analyst | $70,000–$95,000 | ~$82,000–$88,000 | Multi-site exposure, policy refreshes delivered, audit readiness wins |
| Senior/Lead (7–10 yrs) | Senior RHIA, Information Governance Lead, CDI/Coding Ops Lead | $90,000–$115,000 | ~$102,000 | Enterprise KPIs, cross-functional programs, measurable denials reduction |
| Management/Director | HIM Manager/Director, Privacy Manager, Data Governance Manager | $95,000–$140,000+ | ~$115,000–$125,000 | Team leadership, budget ownership, system-level policy and outcomes |
Ranges reflect base pay. Many roles add 3–12% in bonuses, differentials, or stipends depending on setting and policy.
RHIA Salary by organization size (how it usually plays):
- Small facilities (critical access, single-site): pay lands at the lower band. Upside: broader scope, faster title growth.
- Mid-sized hospitals and IDNs: steady mid-to-high placement; complexity and shared services widen ranges.
- Large, integrated systems: consistently high bands. Enterprise policies, larger teams, and KPI ownership lift comp.
Specialty emphasis and pay trend vs. RHIA average
| Specialty emphasis | Trend vs. average | Why it pays | Signals that boost offers |
| Data governance / analytics | Above average | Interoperability, AI-readiness, data quality KPIs | SQL/BI literacy, data lineage, stewardship playbooks |
| Privacy / security | Above average | Regulatory pressure, incident response, risk mitigation | HIPAA/HITRUST frameworks, risk assessments, breach drills |
| CDI / coding operations | Mid-to-high | Revenue impact, denials prevention, quality scores | CDIP, audit throughput, coder productivity gains |
| Payer / vendor / consulting | Mid-to-high | Broader scope, client delivery, travel premiums | Implementation wins, interoperability (HL7/FHIR), stakeholder management |
Quick cues to place yourself fast:
- If you manage people, budgets, or enterprise policies, expect the upper half of the range for your stage.
- Urban/HCOL markets, academic centers, and large IDNs typically add a premium.
- Concrete wins speak loudly: audit pass rates, turnaround-time cuts, data quality lifts, or denials reductions.
Rhia Salary per hour (how to estimate)
You can ballpark your hourly rate in under a minute. Then refine it with your actual schedule, bonuses, and differentials.
- Fast math:
- Hourly = Annual Salary ÷ 2080 (40 hours/week × 52 weeks)
- If your organization uses a 37.5-hour standard week, use 1950 hours instead:
- Hourly (37.5-hr wk) = Annual Salary ÷ 1950
- Part-time? Swap in your own annual hours (weekly hours × 52)
- Examples:
- $65,000 ≈ $31.25/hr
- $85,000 ≈ $40.85/hr
- $100,000 ≈ $48.10/hr
- Note: The quick cuts above are approximations. The table below shows precise 2080-hour calculations rounded to cents.
| Annual RHIA Salary | Hourly (2080 hrs) | Hourly (1950 hrs) |
| $55,000 | $26.44 | $28.21 |
| $65,000 | $31.25 | $33.33 |
| $70,000 | $33.65 | $35.90 |
| $80,000 | $38.46 | $41.03 |
| $85,000 | $40.87 | $43.59 |
| $90,000 | $43.27 | $46.15 |
| $95,000 | $45.67 | $48.72 |
| $100,000 | $48.08 | $51.28 |
| $110,000 | $52.88 | $56.41 |
| $120,000 | $57.69 | $61.54 |
| $140,000 | $67.31 | $71.79 |
- Caveats:
- Many RHIA roles are salaried/exempt. Overtime may not apply; check policy and FLSA status.
- If non-exempt, overtime is typically 1.5× your base hourly after 40 hours/week. Example: $43.27 base → ~$64.91 OT.
- Shift differentials and on-call stipends (evenings/weekends) can lift your effective hourly rate.
- Bonuses matter. A 7% bonus on $90k raises total comp to ~$96,300, which nudges effective hourly upward.
- Remote roles may use geo-based pay bands. Confirm which band applies to your location—and get it in writing.
Tip to nail your own number:
- Start with base hourly using 2080 or your actual annual hours.
- Add known extras (bonus %, differentials, expected OT) to get an effective hourly: (Base Pay + Bonus + Stipends + OT Pay) ÷ Total Hours.
- Rhia Salary by state (tiered overview)
- Tier 1 (often highest-paying, typically urban/HCOL):
- California, Washington, Massachusetts, New York, New Jersey, Washington DC (district), Maryland
- Tier 2 (strong markets with balanced COL):
- Colorado, Virginia, Illinois, Minnesota, Pennsylvania, Connecticut, Oregon
- Tier 3 (solid demand, moderate ranges):
- Texas, Georgia, North Carolina, Arizona, Florida, Ohio, Michigan, Wisconsin, Missouri
- Tier 4 (lower COL, often lower nominal pay but similar purchasing power):
- Indiana, Iowa, Kansas, Nebraska, Kentucky, Tennessee, Alabama, Oklahoma, Arkansas, New Mexico, Louisiana, Mississippi, South Dakota, North Dakota, West Virginia
- Notes:
- Metro > state average: big cities can pay above the state baseline
- Rural facilities may trade lower pay for broader responsibility and faster promotion paths
Use the tiers to zero in on reality fast. Pick your state’s tier, match your career stage, then nudge up or down for your exact metro and scope.
To increase your chances of passing the RHIA exam on the first attempt, many professionals rely on trusted RHIA exam question banks that provide real exam-like questions and answers.
What these tiers typically pay (RHIA-qualified individual contributors)
| Tier | Typical base range | Common midpoint | Approx hourly at midpoint | State/metro examples |
| Tier 1 | $82,000–$115,000 | ~$95,000–$100,000 | ~$45.70–$48.10/hr | CA (SF/LA), WA (Seattle), MA (Boston), NY/NJ (NYC), DC/MD |
| Tier 2 | $75,000–$102,000 | ~$86,000–$90,000 | ~$41.35–$43.30/hr | CO (Denver), VA (NoVA), IL (Chicago), MN (MSP), PA (Philly) |
| Tier 3 | $68,000–$95,000 | ~$78,000–$84,000 | ~$37.50–$40.40/hr | TX (DFW/Austin), GA (Atlanta), NC (RDU), AZ (Phoenix), FL (Miami) |
| Tier 4 | $60,000–$85,000 | ~$70,000–$75,000 | ~$33.65–$36.05/hr | IN, IA, KS, NE, KY, TN, AL, OK, AR, NM, LA, MS, SD, ND, WV |
Notes to use this table well
- These are common bands for RHIA-aligned individual contributor roles (analyst, coordinator, specialist, generalist). Management lifts the range ~10–25% depending on team size and scope.
- Within a state, large academic centers, IDNs, payers, and vendors tend to price at the top quartile. Community hospitals and small ambulatory groups sit mid-band.
- Hourly figures assume 2,080 hours/year and exclude differentials and bonuses.
State and metro callouts (quick reality checks)
- California: Bay Area and LA/OC often land near the top of Tier 1; inland metros sit mid-band.
- Washington & Oregon: Seattle pushes Tier 1 highs; Portland sits upper Tier 2.
- Massachusetts & New York: Boston and NYC metro pay high but COL is steep; upstate NY is more Tier 2–3.
- New Jersey & Maryland: North/Central NJ (NYC-adjacent) and MD near DC track Tier 1; southern areas trend a band lower.
- DC (district): Federal locality pay and consulting presence keep rates strong; verify geo-banded remote policies.
- Colorado & Virginia: Denver/Boulder and Northern Virginia price upper Tier 2; other metros sit mid-band.
- Texas, Georgia, North Carolina, Arizona, Florida: Big metros (DFW, Austin, Atlanta, RDU, Phoenix, Miami) push toward Tier 3 highs; suburban/rural markets price mid-band with faster growth paths.
- Midwest (IL, MN, OH, MI, WI, MO, IN, IA, KS, NE): Chicago and MSP can rival Tier 2; many other metros are Tier 3–4 with solid purchasing power.
How to estimate your number in any state (fast)
- Identify your tier from the lists above.
- Match your stage:
- Early career: aim at the lower third of the tier.
- Mid-career: center on the midpoint.
- Senior IC: target the upper third.
- Add or subtract 5–15% for metro effect:
- +10–15% for top metros in your tier; −5–10% for rural.
- Convert to hourly if helpful: Hourly ≈ Base ÷ 2080.
Tip: Remote roles and geo pay
- National-band employers may pay the same across states; others adjust to your home address. Ask early, confirm in writing, and factor benefits (bonus target, retirement match, CEU funds) into your decision.
Roles and titles that hire RHIA (and typical pay impact)
Here’s how common RHIA-friendly titles map to scope and pay in 2025. Use this to target roles that match your skills and your salary goals.
| Role / Title | Core scope (what you move) | Typical 2025 base | What lifts pay | Common settings |
| HIM Analyst / Specialist (aka Medical Records Analyst, ROI Specialist) | Chart integrity, release-of-information (ROI), edits/flags, data quality fixes. | $60,000–$80,000 | • Epic/Cerner proficiency • Measurable TAT gains • Audit-ready file control | Hospitals, ambulatory groups, outsourcing vendors |
| RHIA (generalist) in hospital/health system | Day-to-day HIM operations, policies, releases, audit prep, KPI tracking. | $70,000–$90,000 | • Multi-site exposure • Accreditation cycles (TJC/DNV) • Cross-team workflow fixes | Community hospitals, IDNs |
| Privacy or Compliance Analyst (healthcare) (HIPAA/GDPR support, incident intake) | Risk assessments, incidents, PHI reviews, policies, training support. | $75,000–$95,000 | • CHPS path • Incident response drills • Audit remediation proof | Hospitals, payers, academic centers |
| Privacy or Compliance Manager (Privacy Officer track) | Program ownership, breach management, education, vendor risk, KPIs. | $95,000–$125,000 | • HITRUST/ISO exposure • Enterprise policy library • Team leadership | IDNs, payers, large clinics |
| Data Governance Analyst (Data Quality, Stewardship Analyst) | Metadata, master data, lineage mapping, data quality rules, BI handoff. | $80,000–$105,000 | • SQL/BI literacy • HL7/FHIR basics • Interop project wins | Health systems, payers, health tech |
| Information Governance Lead (Data/IG Lead, Stewardship Lead) | Enterprise IG councils, policy lifecycle, retention, access governance. | $100,000–$120,000+ | • System-wide scope • Regulatory depth • Tooling rollout (catalog/MDM) | Large systems, academic centers, payers |
| HIM Manager / Department Manager | People, budget, vendors, coding/ROI/document integrity, 24/7 ops. | $95,000–$120,000 | • Team size >10 • Multi-site coverage • Strong KPI ownership | Hospitals, IDNs, specialty networks |
| Director of HIM / Health Information Management | Strategy + compliance across coding, release, privacy alignment, audits. | $120,000–$150,000+ | • Enterprise remit • Budget stewardship • Accreditation success | Large systems, academic medical centers |
| Payer, vendor, or consulting roles (Interoperability, data quality, implementations) | Client delivery, data remediation, governance builds, go-live leadership. | $90,000–$125,000 (+ bonus potential) | • Travel/client-facing • HL7/FHIR fluency • PM skills (PMP/Agile) | Payers, EHR/health tech vendors, consulting firms |
Ranges reflect common base salaries for RHIA-aligned roles in 2025; local markets and system size shift bands. Leadership and vendor/payer roles often include 5–15% bonus targets.
While RHIA certification focuses on health information management, other credentials like Epic certification are also highly valued in healthcare IT, often complementing an RHIA professional’s career path.
Role-by-role quick tips:
- Want faster jumps? Own a metric. Examples: “ROI TAT from 7.2 → 3.8 days,” “Duplicate MRN rate down 42%,” “Closed 100% of access audits monthly.”
- Credentials that pair well:
- Privacy/Compliance → CHPS
- Data/IG → CHDA (plus light SQL/BI)
- Documentation/Coding Ops → CDIP
- Remote-leaning picks: privacy, data governance, payer/vendor delivery. On-site-leaning: HIM operations leadership in acute care.
- Title synonyms to watch in postings:
- HIM Analyst = Clinical Data Integrity Analyst, Medical Records Analyst
- Data Governance Analyst = Data Quality Analyst, Stewardship Analyst
- Director of HIM = HIM Director, Medical Records Director
Choose a lane that fits your strengths, then stack one high-impact skill that the lane pays for.
Settings and how they affect Rhia Salary
How the workplace pays you back—base, bonus, differentials, and growth, depends heavily on setting. Here’s a quick, practical map.
| Setting | Typical Base (2025) | Bonus / Differentials | Remote / Hybrid | Skills that lift pay | Common RHIA-aligned titles |
| Acute care hospitals, AMCs | ~$75k–$120k (Mgr/Dir can reach $140k+ in majors) | Shift/weekend differentials in 24/7 ops; small to mid bonuses | Mostly on-site or hybrid (policy/analytics can be hybrid) | Release-of-information KPIs, CDI/coding oversight, HIPAA/HITRUST, audit readiness | HIM Manager, Director of HIM, Privacy/Compliance Manager |
| Integrated delivery networks (IDNs) | ~$80k–$130k (enterprise roles trend high) | Annual bonuses more common; on-call for enterprise incidents | Hybrid common; some roles travel to sites | Multi-entity governance, data quality programs, EHR standardization, KPI ownership | Information Governance Lead, System HIM Manager, Data Governance Analyst |
| Payers & health tech vendors | ~$85k–$125k base (plus variable); senior product/consulting can exceed | Performance bonuses, sometimes equity; travel stipends | Often remote; geo-based bands may apply | Interoperability (HL7/FHIR), data governance at scale, privacy by design, analytics/BI fluency | Implementation Analyst, Data Governance Manager, Privacy Analyst, Solutions Consultant |
| Outpatient / ambulatory | ~$60k–$90k (fast lift with added scope) | Limited bonuses; occasional productivity incentives | Hybrid possible; on-site for clinic support | Workflow optimization, small-team leadership, payer rules, denials reduction | HIM Supervisor, Clinic HIM Manager, Privacy/Compliance Specialist |
| Government & public health | ~$65k–$100k (grade/step + locality pay) | Robust benefits, pensions; smaller bonuses | Hybrid growing; security-sensitive roles on-site | Regulatory compliance, records retention, incident response, public data reporting | Health Information Administrator, Privacy Officer (local/state), Records Program Manager |
Bold takeaways by setting:
- Acute care hospitals and academic medical centers
- Pay signal: Higher complexity → higher bands. Teaching hospitals and Level I trauma centers tend to pay more.
- What moves the needle:
- Lead ROI turnaround, coding quality, and audit prep for accreditation cycles.
- Own policy overhauls that cut denials or release-of-information errors.
- Expect:
- 24/7 operations; differentials for evenings/weekends in some roles.
- Hybrid is possible for governance and analytics; frontline HIM tends to be on-site.
- Aim for: Concrete KPIs (audit pass rates, DNFB reduction, query response time) in your resume.
- Integrated delivery networks (IDNs)
- Pay signal: Multi-entity governance raises scope and salary. Enterprise roles sit mid-to-high.
- What moves the needle:
- Standardize metadata, retention, and disclosure workflows across facilities.
- Drive EHR build consistency and data quality measures system-wide.
- Expect:
- Program ownership, cross-site steering groups, occasional travel.
- Bonuses tied to system metrics and adoption milestones.
- Aim for: Language around “enterprise policy,” “multi-site rollout,” and “governance council.”
- Payers and health tech vendors
- Pay signal: Competitive base + variable comp. Analytics and interoperability skills pay premium.
- What moves the needle:
- Fluency in HL7/FHIR mappings, payer data quality, and privacy-by-design reviews.
- Client-facing delivery, solution configuration, or implementation leadership.
- Expect:
- Remote-first culture; geo-banded pay. Travel for go-lives or client workshops.
- Clear performance bonuses and sometimes equity at vendors.
- Aim for: Measurable outcomes—reduced rework, smoother integrations, faster time-to-value.
- Outpatient and ambulatory settings
- Pay signal: Moderate base; quick responsibility growth as you wear multiple hats.
- What moves the needle:
- Optimize front-to-back documentation, prior auth, and denials workflows.
- Stand up simple dashboards for turnaround time, chart completion, and release accuracy.
- Expect:
- Lean teams; you can become “the” HIM person quickly.
- Hybrid often feasible once processes stabilize.
- Aim for: Show before/after metrics from small process changes that saved hours or dollars.
- Government and public health
- Pay signal: Stable pay with strong total comp (benefits, retirement). Salary follows grade/step + locality.
- What moves the needle:
- Master records management, FOIA/PRA workflows, and incident response playbooks.
- Translate regulatory updates into practical SOPs and training.
- Expect:
- Predictable schedules; promotion via formal ladders.
- Hybrid policies vary by agency and data sensitivity.
- Aim for: Certifications (e.g., CHPS) plus clear compliance outcomes in audits and investigations.
Mini-calculator for fit:
- Want highest ceiling? Consider IDNs, payers, or large AMCs. Pair RHIA with CHPS, CHDA, or CDIP.
- Want rapid scope and title growth? Ambulatory groups and community hospitals move fast.
- Want stability and strong benefits? Government/public health wins—all about grade/step and locality.
- Want remote flexibility? Vendors and payers lead; governance/analytics roles in providers are next.
Tip: Regardless of setting, bring numbers. A one-line win like “Cut ROI turnaround from 7.2 to 3.8 days” travels well across markets and lifts your RHIA salary talks.
What drives RHIA compensation most
Comp follows impact. Show bigger, repeatable wins, and pay follows you. These are the levers that consistently move Rhia Salary bands.
Experience depth
- Make complexity your calling card. Examples that travel well:
- EHR transitions and optimizations (Epic/Cerner/Meditech), including data conversion and chart completion playbooks
- Multi-site governance: standardizing HIM policies across hospitals, clinics, and ancillaries
- Audit readiness: Joint Commission, CMS, OCR—clean findings, tight corrective actions
- Accreditation cycles with measurable outcomes (deficiency rate drop, faster closure)
- M&A integrations: record retention alignment, MPI consolidation, HIM workflow harmonization
- Hiring signals that land:
- “Cut DNFB from 5.2 to 3.1 days across 3 hospitals in 2 quarters”
- “Led OCR incident response tabletop; closed gaps within 45 days; no CAP issued”
- Tip: stack 2–3 complex wins. One-off wins help; patterns pay.
While RHIA certification focuses on health information management, other credentials like Epic certification are also highly valued in healthcare IT, often complementing an RHIA professional’s career path.
Scope and scale
- Pay scales with ownership. Team size, budget, and KPIs matter more than title labels.
- Scope milestones that typically move bands:
- Own a KPI (ROI turnaround, chart deficiency rate, duplication rate, release accuracy)
- Lead cross-functional programs (HIM x Rev Cycle x IT x Privacy)
- Manage people and processes (supervisors, analysts, coders; on-call; vendor SLAs)
- Write/maintain enterprise policy and measure adherence
- Quick ladder snapshot:
- Individual contributor with enterprise influence > standard IC
- Manager of 5–12 FTE > lead without FTEs
- Multi-site or system-level manager > single-facility manager
- Director with KPI portfolio and budget > narrow-scope director
Specialized skills
- Privacy/security frameworks: HIPAA/HITRUST, risk analysis, incident response, BAAs, minimum necessary
- Data governance: data lineage, master data/MPI strategy, metadata cataloging, stewardship councils
- CDI/coding operations: DRG/HCC alignment, denials prevention, query governance, coder QA
- Interoperability: HL7 v2, FHIR, APIs, TEFCA/readiness, info blocking workflows, release-of-information automation
- Analytics fluency: SQL fundamentals, BI tools (Power BI/Tableau), KPI design, data definitions
- Evidence beats adjectives. Show queries, dashboards, or SOPs you built, redacted if needed.
If you’re exploring different credentials in the healthcare field, you can check out a full list of healthcare certifications that can boost your career opportunities.
Credentials and education
- RHIA is the baseline; targeted add-ons lift confidence (and bands) when tied to scope:
- CHPS (privacy/security) → strongest for privacy, compliance, and risk roles
- CDIP (documentation improvement) → CDI leadership and revenue integrity adjacencies
- CHDA (data analytics) → governance/analytics roles, vendor/payer analytics teams
- MHA/MHI → leadership ceiling and faster promotion; pair with measurable outcomes
- Bonus signals: Lean Six Sigma (process improvement), project credentials (CAPM/PMP) for large implementations
Market forces
- Geography: urban teaching hospitals, West Coast/Northeast, DC metro, and vendor/payer hubs pay more
- Employer type: payers, consulting, and health tech vendors often run mid-to-high due to scope, travel, and bonus structures
- Regulatory waves lift pay: info blocking enforcement, state privacy laws, TEFCA, cybersecurity frameworks
- Timing matters: EHR consolidation, shared services launches, and data modernization projects unlock higher bands
Quick proof > long narratives
- Convert work to math:
- “Reduced duplicate MRN rate from 3.2% → 0.9% in 6 months (MPI stewardship + training)”
- “Automated ROI status dashboard; cut backlog by 42%”
- “Improved chart completion compliance from 86% → 97% within 90 days; avoided suspension events”
- Interview formula:
- Situation → Action → Metric → Business outcome (cash flow, audit, patient safety, compliance risk)
| Compensation lever | Proof employers trust | How to signal it | Typical effect |
| Experience depth | EHR go-live/optimization, multi-site policy rollouts, accreditation wins | 1–2 quantified case studies with dates, systems, and outcomes | Moves you from low → mid or mid → high in band |
| Scope and scale | FTE leadership, KPI ownership, enterprise policy authority | Resume line with team size, KPIs, budget/vendor oversight | Largest driver; often the step between bands |
| Specialized skills | HIPAA/HITRUST, HL7/FHIR, CDI governance, SQL/BI portfolios | Short skill stack + artifact links (dashboards/SOPs) | Shifts you to upper third when aligned to role |
| Credentials & education | RHIA + CHPS/CDIP/CHDA; MHA/MHI for leadership lanes | Place after your name; add “used to achieve X metric” | Cred boost; accelerates promotion and range entry |
| Market forces | Urban/HCOL markets, vendor/payer demand, regulatory shifts | Note geo bands; compare base + bonus + COL | Sets the ceiling/floor for your band |
Practical ways to “show the money” in RHIA roles
- ROI turnaround: median ≤ 3 business days; accuracy ≥ 99.5%; zero PHI spillage
- DNFB and chart deficiencies: -30% within 2 quarters; clear SLA with medical staff
- Privacy incidents: reduce per 1,000 encounters; documented risk analysis and closure time
- Data quality: duplicate MPI rate < 1%; automated merge workflow with audit trail
- Interop: FHIR endpoint uptime > 99.9%; info blocking requests fulfilled within policy window
- Analytics: single source of truth for HIM KPIs; adoption by Rev Cycle and Compliance
Fast impact math (use in negotiations and reviews)
- “Cut 2 DNFB days” × “$1.5M/day average cash” ≈ $3M cash flow lift; small improvements, huge value
- “-40% ROI backlog” + “-25% payer denials tied to documentation” = measurable labor and revenue upside
- Tie your ask to outcomes. Short, numeric, defensible.
Bottom line
- Depth proves you can handle complexity.
- Scope proves you can scale it.
- Skills and credentials open doors.
- Market sets the outer limits.
Stack them, show receipts, and your Rhia Salary finds the high end of the band.
How to increase your Rhia Salary in 6–12 months
You don’t need a new job to earn more. You need clearer impact and receipts. Make your value easy to see, then point to it.
How to Grow Your RHIA Career Scope
Earning the RHIA credential is a powerful first step, but growth comes from showing impact where you are. That doesn’t always mean waiting for a big promotion, sometimes the fastest way to stand out is to own metrics, lead small projects, sharpen niche skills, and make your results visible. Here’s how to expand your scope and influence as an RHIA in 2025.
1. Own a Metric That Matters
Leaders pay attention to numbers. Volunteering to take charge of one metric not only shows initiative but also proves your ability to drive measurable results.
Examples of metrics you can take on:
- Release-of-information (ROI) turnaround times (meeting SLAs)
- Discharged, not final billed (DNFB) days
- Coding backlog or rework rates
- Duplicate medical record numbers (MRNs)
- Audit findings closed on time
Quick wins to aim for:
- Cut ROI turnaround by 15–20% by standardizing request triage and tightening handoffs.
- Reduce coding rework with a two-step queue and a clear “definition of done.”
- Lower duplicate MRNs by running a weekly data stewardship huddle with defined merge criteria.
Micro-script to propose ownership:
“I’d like to own [metric] for the next quarter. Goal: move from [baseline] to [target]. I’ll send a weekly one-pager and share blockers early.”
2. Lead a Mini Governance or Policy Project
Even small-scale governance work shows you can think cross-functionally and mitigate risk.
Starter projects:
- Refresh ROI policy with current state regulations
- Update and streamline data access roles
- Create a simple data dictionary for 10 high-use fields
Deliverables that make an impact:
- Current vs. future process maps
- A clear RACI (responsibility matrix)
- A 90-day follow-up with measurable outcomes
3. Sharpen High-Value Skills
Investing in skills beyond the basics makes you the go-to resource.
Privacy & Security
- Learn: HIPAA Security Rule, risk analysis, incident response steps
- Build: a one-page incident playbook and “evidence locker” checklist
- Practice: shadow a real or simulated incident, timing your response
Data Quality & Governance
- Learn: stewardship roles, data quality dimensions (accuracy, completeness, timeliness)
- Build: a lightweight data dictionary + scorecard for 3–5 data elements
- Run: monthly duplicate resolution sprints, publishing before/after metrics
Interoperability & Analytics
- Learn: HL7 ADT message segments; FHIR resources (Patient, Encounter, Observation)
- Build: SQL queries to track coding turnaround or ROI SLAs; visualize results in Power BI/Tableau
- Translate: turn interface errors into clear “what/why/fix” summaries for operations teams
4. Add Targeted Credentials
Stacking the right credentials can accelerate advancement. Choose one that complements your current role:
- CHPS – privacy and security
- CDIP – documentation improvement
- CHDA – data analytics
How to approach it:
- Plan a 10–12 week sprint with weekly study sessions and practice questions
- Create an “evidence of learning” artifact (e.g., risk assessment template for CHPS, query playbook for CDIP, dashboard with KPIs for CHDA)
5. Keep Your RHIA Visible
Make sure the credential works for you every day:
- Update LinkedIn, email signature, and resume headline: RHIA + target credential in progress
- Log CEUs consistently
- Share short posts about completed courses with real micro-outcomes
6. Do a Market Check
Don’t wait until review season to understand your value.
How to prepare:
- Collect 3–5 job postings that match your scope (team size, systems, KPIs)
- Map your deliverables against their requirements
- Build a one-pager for reviews: “Role-market match,” your metrics, and a realistic salary range
Typical outcomes: merit increase, mid-cycle adjustment, or fast-track promotion.
7. Network With Purpose
Connections open doors. Show up and share wins where it matters.
Steps to take:
- Join your local AHIMA component; attend one CSA meeting each quarter
- Volunteer for a short lightning talk (5–7 minutes) or present a quick win poster
- Post a 150-word LinkedIn update on a metric you improved and how you did it
- Build two warm recruiter relationships and set alerts for the next-level roles you’re targeting
| Timeframe | Move | Deliverable | Evidence/KPI | Leverage in Comp Talk | Effort |
| Weeks 1–4 | Own one KPI (ROI, DNFB, coding backlog) | Baseline + target + weekly one-pager | e.g., ROI SLA 78% → 90% | “I led a measurable improvement in HIM operations.” | 2–3 hrs/week |
| Weeks 5–8 | Mini governance project | Updated policy or data dictionary (10 fields) | Fewer escalations; audit-ready evidence list | “Reduced risk and clarified roles across departments.” | 3–4 hrs/week |
| Weeks 9–12 | Skill sprint (CHPS/CDIP/CHDA-aligned) | 1 artifact: incident playbook, query guide, or dashboard | Checklist complete; dashboard live with definitions | “I brought new capability we now use weekly.” | 3–5 hrs/week |
| Months 4–6 | Credential in motion | Exam scheduled + study log + practice scores | ≥70–80% on practice; CEUs logged | “Ready for larger scope; credential timeline set.” | 2–4 hrs/week |
| Months 5–6 | Market check | One-page market brief (5 roles, ranges, scope match) | Title vs. scope mapping; range target | “Here’s evidence my scope aligns with [range].” | 1–2 hrs total |
| Months 6–12 | Show and tell (networking) | CSA lightning talk + LinkedIn case study | Slides + public post with metrics | Recruiter interest; internal visibility; promo-ready | 1–2 hrs/month |
Helpful proof points to track (you’ll use these in reviews and interviews):
- Before/after metrics with dates and sample size
- Process maps or checklists you authored
- Dashboards or queries with clear definitions
- Policy updates with approvals and training sign-offs
- Cross-functional emails or meeting notes showing you drove the change
Expected outcomes when you execute consistently:
- In-place raise or title adjustment (often 5–12% for scope growth; more with promotion)
- Stronger offers externally (interviews flow easier when your wins are quantified)
- Faster path to manager/lead scope (even in smaller markets)
Keep it simple, visible, and repeatable. One metric. One project. One skill. Then stack.
Security, Work Patterns, and Salary Negotiation for Remote RHIAs
Remote and hybrid roles have become the norm for many RHIAs, but expectations around security, compliance, and pay negotiation are evolving quickly. To succeed, professionals need to understand both the technical requirements of remote work and the strategies to secure fair compensation.
Security and Compliance Expectations
Must-Haves:
- Encrypted device
- Multi-factor authentication (MFA)
- Virtual desktop infrastructure (VDI) access
- Privacy screen
- Lockable workspace
- Written PHI handling procedure (printing, storage, shredding)
- Regular security training and attestations
Nice-to-Haves:
- Hardware token (e.g., FIDO2)
- Data loss prevention (DLP) monitoring
- Session timeouts
- Zero-trust access
Green flag from employers:
- Company-provided equipment
- Internet stipend
- Documented incident response plan
Common Hybrid Work Patterns
- 4–1 model: Four days remote, one day on-site for team syncs and provider touchpoints
- 3–2 model: On-site Tuesday/Thursday for committees, plus one flex day as needed
- Remote-first with quarterly on-sites: Planning, audits, and cross-functional sessions
- Travel-based vendor roles: Primarily remote with 10–25% travel for implementations
Quick Role Evaluation (5-Minute Checklist)
Before applying, check if the posting clearly states:
- Work mode (remote, hybrid with days, or fully on-site)
- Core hours and time zone alignment
- Equipment, stipend, and security requirements
- Pay band and geographic pay policy
- Measurable outcomes tied to the role (KPIs, SLAs, audit targets)
Script to clarify expectations:
“To align expectations, can you confirm the work mode (remote/hybrid), the geo-based pay policy you use, and the zone or hub this role maps to? I’m happy to share my location for accurate banding.”
Building a Strong Salary Case
Your negotiation will land best when tied to outcomes, not just market charts.
Proof points to highlight:
- Audit readiness: fewer findings, clean corrective actions, on-time submissions
- Denials & documentation: lower avoidable denials, improved physician query response times
- Release of information: faster turnaround, higher accuracy
- Data governance: stronger policy adoption, better quality scores, reduced backlog
Market prep:
- Collect 3–5 postings that match your scope (team size, KPIs, systems)
- Note pay bands and location
- Build a one-page “role-market match” for review discussions
Set a target range:
- Example: “Given enterprise governance scope and team leadership, I’m targeting $90k–$100k base.”
- Add 2 non-salary levers (bonus, CEU budget, remote flexibility) to leave room for trade-offs
Negotiation Scripts
30-Second Phone/Zoom Anchor
“Thanks for the offer. I’m excited about the role and the impact—especially the EHR optimization and ROI accuracy goals. Based on market data and the scope we discussed, I’m targeting a base in the $90–$100k range. If we can align there and include CEU/certification support, I can accept promptly.”
Polite Email Template
Subject: Offer details and quick alignment
“Hi [Name], I’m thrilled about the RHIA-aligned role and the chance to drive [2–3 KPIs]. Based on current ranges for similar scope and the outcomes I can deliver in the first two quarters, I’m targeting $90,000–$100,000 base. Could we explore that band, along with a 5–10% bonus target and certification reimbursement (RHIA/CHPS/CDIP CEUs)? If we can align, I’m ready to sign this week. Thank you for considering.”
Negotiation Levers to Consider
Beyond Base Salary:
- 5–10% bonus target with defined metrics
- CEU budget ($1k–$2k), exam fees, study time
- Remote work flexibility, on-call stipends, shift differentials
- Extra PTO or floating holidays
- Title calibration (Manager vs. Lead) to match scope
- Written 6-month comp review tied to defined outcomes
If salary maxes out:
- Request a sign-on bonus to bridge the gap
- Negotiate a 6-month review with clear KPI-based path to higher pay
- Adjust title to better reflect enterprise scope, unlocking higher bands later
Internal Raise Mini-Script
“In the last 6 months I reduced [KPI] by X% and led [project] across Y departments. Market for this scope sits around $85k–$95k. I’m requesting an adjustment to $90k and am happy to document goals tied to a follow-up review.”
Quick Do’s and Don’ts
Do:
- Tie negotiation to scope, scale, and KPIs
- Use salary ranges, not single numbers
- Be ready to sign if aligned
Don’t:
- Issue ultimatums
- Over-explain
- Lean on vague “cost of living” arguments without role scope evidence
Bottom line: For remote RHIAs, the strongest position combines security readiness, clear role expectations, and outcome-based proof points. When you enter negotiations prepared, you don’t just ask for a number, you make the case for your value.
| Pay policy type | How it works | Common where | RHIA impact | Questions to ask |
| National single band | Same range nationwide | Vendors, larger payers | Predictable; good for remote candidates in lower-COL areas | “What’s the national midpoint and bonus target?” |
| Geo‑zoned bands | High/med/low COL zones adjust pay | Health systems, gov’t | Your address sets the band; moving can reprice your salary | “Which zone am I in and what triggers a reband?” |
| Hub/anchor‑city pricing | Paid as if located in a named hub | Consultancies, multi‑site IDNs | Often better than local pay if your hub is high‑COL | “Which hub applies to this requisition?” |
| Local market bands | Tied to hiring facility’s city | Hospitals, clinics | Remote allowed, but pay mirrors the facility’s city | “Is pay anchored to the facility location or employee location?” |
| Offer Component | My Target | Employer Offer | Gap | Trade / Ask | Priority |
| Base Salary | $90,000–$100,000 | $86,000 | $4,000–$14,000 | If base capped, add $5k sign-on + 6‑mo review to $92k tied to KPI | High |
| Bonus Target | 8–10% | 5% | 3–5 pts | Increase target or set guaranteed first-year minimum | Medium |
| CEU/Cert Support | $1,500 + exam fees | $500 | $1,000 | Boost CEU budget + paid time for RHIA/CHPS/CDIP maintenance | High |
| Work Model | Hybrid 3/2 or remote | On-site 5 days | Flexibility | Pilot hybrid; clarify geo-pay bands in offer | Medium |
| Title | HIM Manager or Governance Lead | Senior Specialist | Leveling | Title bump to match enterprise scope; enables next band later | Medium |
Career ladders and next steps
- Common paths:
- RHIA → HIM Manager → Director of HIM → System Director
- RHIA → Privacy/Compliance Manager → Privacy Officer
- RHIA → Data Governance Lead → Information Governance Manager
- Crossovers:
- CDI leadership, revenue integrity, payer operations, health tech product roles
What these paths look like in practice
- RHIA → HIM Manager → Director of HIM → System Director
- Prove you can run core HIM operations: release-of-information (ROI) accuracy, turnaround time (TAT), chart completion, deficiency management.
- Then scale it: multi-site policy standardization, audit readiness (TJC, CMS), KPI dashboards, staffing models, budget inputs.
- At Director/System Director, expect enterprise governance, upstream data quality, cross-functional steering groups, and vendor contracts.
- RHIA → Privacy/Compliance Manager → Privacy Officer
- Start with incident intake, risk assessments, breach response timelines, and training compliance rates.
- Move to program ownership: HIPAA/HITECH policy lifecycle, BAAs, OCR audit prep, annual risk analysis, and board reporting.
- Privacy Officer = strategy, enterprise policy, metrics cadence, and liaison with legal, IT security, and executive leadership.
- RHIA → Data Governance Lead → Information Governance Manager
- Begin with data lineage, metadata, retention schedules, and data access workflows.
- Lead stewardship councils, define data quality rules, and reduce duplicate records (MPI) and denials from data defects.
- IG Manager owns the roadmap: policies, master data, interoperability quality (HL7/FHIR), and analytics enablement.
| Ladder step | Scope you’ll handle | Typical 2025 range | Lift vs prior | Fastest boosters |
| RHIA (generalist) | Daily HIM ops, data quality tickets, ROI/TAT monitoring | $70k–$90k | — | Quantify wins, cross-train, take on KPI ownership |
| HIM Manager | Team leadership (coding/ROI/deficiencies), budget inputs, audits | $95k–$120k | +10–25% | Lead a policy refresh; build a dashboard executives use |
| Director of HIM / System Director | Enterprise governance, multi-entity standardization, vendor oversight | $115k–$140k+ | +10–20% | Multi-site wins; board-ready metrics; change management credentials |
| Privacy/Compliance Manager | Incidents, risk assessments, training, OCR readiness | $85k–$110k | +5–20% | CHPS; incident response playbooks; vendor BAA clean-up |
| Privacy Officer | Program strategy, board reporting, enterprise policy | $110k–$140k | +10–25% | Crosswalk HIPAA↔HITRUST; executive communication |
| Data Governance Lead | Stewardship councils, data quality rules, MPI cleanup | $90k–$115k | +5–20% | CHDA; SQL/BI basics; HL7/FHIR familiarity |
| Information Governance Manager | IG policies, retention, access governance, interoperability quality | $105k–$130k | +10–20% | Enterprise roadmap; KPI ownership; change adoption |
| Crossovers (CDI/Revenue Integrity) | Documentation quality, denials reduction, revenue lift projects | $95k–$120k | +10–20% | CDIP; measurable denial rate drops; coder-clinician bridge |
| Crossovers (Payer Ops / Health Tech) | Interoperability, product workflows, implementations, data quality | $95k–$130k | +10–25% | Vendor experience; travel-readiness; API/HL7 fluency |
12‑month moves to climb one rung
- Q1: Pick one metric to own end‑to‑end (e.g., ROI TAT, privacy incident cycle time, duplicate MRN rate). Baseline it.
- Q2: Ship a lightweight dashboard and a monthly review. Document process fixes and outcomes.
- Q3: Lead a mini initiative across at least two departments. Capture approvals, SOPs, and training artifacts.
- Q4: Package results: before/after metrics, ROI, risks retired. Use it to negotiate title/salary or to apply externally.
Portfolio signals that travel
- A one‑pager with 3 KPIs you improved, each with starting value → end value → method.
- A redacted policy refresh or data dictionary snippet you authored.
- A governance council charter or RACI you ran.
- Screenshots (sanitized) of a BI dashboard you built or curated.
Credential map (focused, not random)
- HIM leadership path: RHIA + CDIP (documentation), optional MHA/MHI.
- Privacy path: RHIA + CHPS; add basic HITRUST awareness.
- Data/IG path: RHIA + CHDA; sprinkle SQL/BI and HL7/FHIR basics.
- Crossovers: pair with the domain—CDIP for CDI, CHDA for analytics-heavy vendor roles.
Interview lines that show value
- “We cut ROI turnaround from 5.2 to 2.9 days in 90 days by fixing queue routing and adding a QC check.”
- “I ran the breach response drill quarterly; time‑to‑containment dropped 38% and OCR documentation was audit‑ready.”
- “Our stewardship council reduced duplicate MRNs by 46% and lowered claim edits tied to ID mismatches.”
Tip: Titles vary. Scope sells. When your scope grows (team size, multi‑site policy, enterprise KPIs), Rhia Salary follows.
How to validate numbers and track your market
Use this simple loop to keep your RHIA pay data current and defensible:
- Triangulate from more than one source
- Normalize for scope, location, and benefits
- Log findings, then revisit on a 90‑day cadence
- Check multiple sources:
- Job boards, employer career sites, professional association surveys
- Go wide, then go deep:
- Job boards with posted ranges (filter by “pay transparency” markets: CA, CO, NY, WA)
- Employer career portals (grade/level + posted band = gold)
- AHIMA and local Component Association snapshots
- Public sector pay schedules (state/county health, VA system) for clear bands
- Vendor/payer postings for scope-rich roles (interoperability, data governance)
- What to capture from each listing:
- Title, department, location/hybrid status
- Base range, bonus target, differentials
- Required years of experience, team size, and scope signals (sites, beds, programs)
- Tech stack and regs (EHR, HL7/FHIR, HIPAA/HITRUST, OCR audits)
| Source | What to grab | Freshness | Strength | Watchouts |
| Employer career sites | Exact bands, grade level, benefits | Real-time | Most accurate for that org | Geo-adjusted bands may apply |
| Job boards (pay-transparent states) | Posted base range, title variants | Daily | Large sample sizes | Ranges can be broad; scope varies |
| Association surveys (AHIMA, state) | Median and quartiles by role/region | Annual/biannual | Trusted methodology | Lag vs. current postings |
| Public sector pay tables | Step ranges, COLA updates | Periodic | Clear ladders and benefits | Less flexible on negotiation |
| Vendor/payer/consulting listings | Scope, travel, bonus targets | Real-time | Often higher bands for complexity | Travel/time demands trade-offs |
- Align titles with scope:
- Compare team size, budget, and KPIs, not just the title label
- Normalize titles. “HIM Analyst,” “Information Governance Analyst,” and “RHIA” can sit at different levels depending on:
- Team size and direct reports
- Bed count/sites supported (single hospital vs. IDN)
- Regulatory footprint (HIPAA/HITRUST, audits, OCR activity)
- Program ownership (ROI turnaround, denials reduction, data quality KPIs)
- Tech scope (EHR modules, HL7/FHIR interfaces, BI stack)
- Quick scoring rubric (helps match to a pay band):
- 0–1 points each; add them up:
- Team leadership (0 = none, 1 = ≥5 reports or dotted-line leads)
- Sites/bed count (0 = single/small, 1 = multi-entity or ≥300 beds)
- Program ownership (0 = contributor, 1 = measurable KPI owner)
- Regulatory complexity (0 = routine, 1 = audits/accreditation lead)
- Data/interop scope (0 = basic, 1 = HL7/FHIR/governance oversight)
- 0–1 points: entry–mid. 2–3: solid mid–high. 4–5: senior/manager+.
- 0–1 points each; add them up:
| Score | Likely band (base) | Typical titles |
| 0–1 | $55k–$75k | HIM Analyst, RHIA (early), ROI/Compliance Analyst |
| 2–3 | $75k–$100k | Information Governance Analyst, Privacy Analyst, Senior HIM Specialist |
| 4–5 | $100k–$140k+ | HIM Manager, Data Governance Lead, Director of HIM |
- Re-check quarterly:
- Market shifts with budgets, mergers, and regulatory changes
- Set alerts and a cadence:
- Create saved searches on major boards; weekly digest keeps you current
- Calendar a 90‑day “comp audit” to refresh your range and notes
- Track policy shocks (info blocking enforcement, state privacy laws), EHR upgrades, mergers—these move demand
- Keep a comp log (lightweight works best):
- Columns: Date | Source | Title | Location | Posted Range | Scope notes | Benefits | Link
- Remove outliers (top/bottom 10%) before you average
Practical adjustments that make your number real:
- Geo factor:
- If a posting shows $95,000 in Boston and your org pays national bands with geo-adjustment, a 0.85 cost-of-labor factor suggests ~$80,750 equivalent. Always confirm employer methodology (cost of labor vs. cost of living).
- Benefits and bonus:
- Effective annual = base + expected bonus + typical differentials + employer retirement match value
- Example: $88,000 base + 8% bonus + 4% match ≈ $96,800 total value (before healthcare premiums, tuition aid)
- Hourly estimate (to compare apples-to-apples):
- Hourly ≈ base ÷ 2080. Add differentials/OT only if they reliably occur.
How to triangulate a tight personal range (fast):
- Gather 10–15 relevant postings (same region and scope level)
- Strip out outliers and non-comparable titles
- Take the midpoint of each range; average those midpoints
- Adjust ±5–10% for your specific scope signals (team size, KPIs owned, regulatory complexity)
- Land on a 10k window you can confidently defend in negotiation
Search strings that surface the right roles:
- (“RHIA” OR “Registered Health Information Administrator” OR “HIM Manager”) AND (privacy OR “data governance” OR interoperability OR “information governance”)
- Add location filters or “remote” + “health system,” “payer,” or “vendor” to see varied bands
Stay ethical and current:
- Use official, current postings and association data; cite them in conversations
- Screenshot or save PDFs, postings change or expire
- Confirm geo-based pay practices early and get final numbers in writing before you accept
RHIA credential: official info and pathways
Thinking about RHIA? Here’s the clean, official path so you can move fast and stay compliant.
What RHIA validates
- Enterprise HIM leadership, data governance, privacy/security oversight, analytics enablement, and regulatory compliance across care settings.
- Issued by AHIMA. Recognized by hospitals, IDNs, payers, and health tech vendors.
Who’s eligible (official pathways)
- You qualify to sit for RHIA via a CAHIIM-accredited HIM program. Pick the route that matches your background.
| Pathway | Best for | Time to qualify | Core actions |
| CAHIIM-accredited HIM Bachelor’s | Students or career-changers ready for a full undergrad program | ~4 years (varies by transfer/AP credits) | • Enroll in a CAHIIM-accredited HIM BS program • Complete required coursework + any practicum • Apply to AHIMA and schedule your exam |
| CAHIIM-accredited HIM Master’s | Professionals with a bachelor’s seeking advanced preparation | ~1–2 years (program dependent) | • Enter a CAHIIM-accredited HIM MS/MHI/MHIIM program • Finish degree requirements • Register with AHIMA and take RHIA |
| CAHIIM-accredited Post‑Bacc Certificate | Bachelor’s holders needing HIM-specific competencies for RHIA eligibility | ~9–18 months (intensive, focused) | • Complete a CAHIIM-accredited post‑bacc HIM certificate • Confirm eligibility with AHIMA • Book your exam date |
Important: The older RHIT‑to‑RHIA “proviso” pathway has ended. Today, RHIA eligibility routes through CAHIIM-accredited programs. Always verify accreditation status before enrolling.
How the exam works (at a glance)
- Computer-based, multiple-choice, delivered via authorized testing centers (e.g., Pearson VUE) or approved online proctoring.
- Content spans: data governance and quality, information protection/privacy/security, informatics/analytics and data use, revenue cycle/compliance, and leadership/strategy.
- Includes unscored pretest items. Exact counts, timing, and current policies live on AHIMA’s site.
Before taking the official test, it’s a smart idea to try a free RHIA practice exam to evaluate your readiness and identify areas that need improvement.
Maintaining your RHIA
- Recertify on AHIMA’s cycle with continuing education units (CEUs). RHIA typically requires 30 CEUs every 2 years, including an ethics CEU. Check AHIMA for current totals, category limits, and fees.
- Keep CEUs aligned to your role focus (privacy, governance, analytics). This keeps you exam‑current and promotion‑ready.
Smart picks if you plan to “stack” credentials
- CHPS for privacy/security leadership (HIPAA, risk, incident response).
- CDIP for documentation integrity and clinical alignment.
- CHDA for analytics/data storytelling across operations and finance.
- Stack intentionally: choose the one that extends your current scope (and pay band).
How to choose a program
- Verify accreditation: find programs in the CAHIIM directory: https://www.cahiim.org/accredpgms/directory-of-programs
- Scan outcomes: RHIA pass rates, practicum options, employer partnerships.
- Fit your schedule: on‑campus vs. online, cohort pacing, start dates.
- Map to your goal role: leadership-heavy programs help for manager/director tracks; analytics-forward programs fit vendor/payer/data roles.
Mini‑checklist
- Confirm a CAHIIM-accredited pathway fits your timeline.
- Pull the current RHIA Candidate Guide from AHIMA.
- Pick an exam window. Work backward with a weekly study plan.
- Line up CEU plans post‑exam so you never scramble at renewal.
Learn more from AHIMA:
- Certifications overview: https://www.ahima.org/certification-careers/certifications-overview/
Prep and continuing education:
- Vendor-neutral overview and requirements on AHIMA’s site
- Ethical prep and practice questions can speed readiness
Exam prep that supports your salary goals
Strong prep isn’t just about a pass. It proves you can run governance, protect privacy, and move data quality metrics—exactly what hiring managers pay for.
- Why prep matters for pay:
- Earning RHIA (and add‑ons like CHPS/CDIP/CHDA) expands your role scope, which directly lifts compensation.
- Better prep = faster pass = sooner eligibility for higher-band roles and bonuses.
- Where to practice:
- AHIMA vendor page with resources: https://certempire.com/vendor/ahima/
- RHIA-focused practice materials to sharpen weak areas: https://certempire.com/exam/rhia-pdf-dumps/
- Also use official, ethical sources (AHIMA’s outlines, textbooks, and legit mock exams). Avoid any material claiming to be “real exam questions.” That violates AHIMA policy and can risk your credential.
- Smart study moves:
- Use practice questions with clear rationales; prioritize sets that mimic the RHIA blueprint.
- Track domains where you miss items; turn misses into short, searchable micro-notes.
- Schedule the exam date early to create a clean deadline and backward-plan your study.
- Work in sprints (40–60 minutes), review quickly, then switch domains to reduce fatigue.
- Simulate test day weekly: timed blocks, no notes, single sitting.
Your 6‑week RHIA study plan (simple and punchy)
| Week | Primary domains | Focus & actions | Practice target | Outcome |
| 1 | Information Governance; Leadership | Skim AHIMA blueprint; map domains to KPIs (policies, retention, metrics). Draft 10 micro-notes/day. | 100 questions, untimed, read every rationale. | Baseline score + gaps list. |
| 2 | Privacy & Security (HIPAA, HITRUST); Compliance | Incident response flow, risk analysis vs. assessment, BAAs, sanctions. Build checklists. | 120 questions, timed (1 min/q). | Close high-risk misses; update micro-notes. |
| 3 | Data Analytics & Use; Data Quality; Interoperability (HL7/FHIR basics) | KPI literacy (validity, completeness), basic SQL/BI terms, metadata and stewardship roles. | 150 questions; 2 mini-mocks (50 each). | Raise timed accuracy to ~70–75%. |
| 4 | HIM Operations; ROI; Documentation; Revenue Cycle overview | Release-of-information workflows, retention schedules, audit readiness, denials basics. | 150 questions; focus on scenario-based items. | Confident with operations scenarios. |
| 5 | Integration & Review (all domains) | Two full-length mocks under exam timing. Post‑test debrief. Patch weak domains. | 2x full mocks (≥ 3 hours each). | ≥ 80% on latest mock or clear plan to close gaps. |
| 6 | Light Review & Exam Readiness | Rehearse tricky flows (breach, subpoenas, access requests). Sleep, hydrate, brief flashcard pass. | 60–80 targeted questions, no cramming. | Calm, consistent recall. |
Quick resource vetting (keep it ethical)
- Look for original practice questions with detailed rationales. No “memory dumps,” no copied items.
- Cross-check topics against the AHIMA RHIA blueprint.
- Favor providers that update content annually and cite standards/regulations.
- When in doubt, ask the vendor to confirm their items are original and policy-compliant.
Set the deadline
- Pick a date 6–8 weeks out. Put it on your calendar. Tell a friend or mentor—light accountability works.
- Book two mock exams on the same weekday/time as your real test.
Last mile tips
- Read every stem carefully; watch for scope words (first, best, most appropriate, policy vs. procedure).
- Eliminate two options fast; compare remaining choices to policy or standard language.
- Breathe. Steady pace beats sprinting.
With a tight plan, ethical materials, and timed practice, you’ll pass sooner, and step into the pay band your skills deserve.
Next Steps!
- Map your target role and location to a realistic range
- Close one skills gap that directly supports scope (privacy, analytics, or governance)
- If you’re pursuing RHIA now, line up ethical practice materials and schedule a date:
- AHIMA vendor resources: https://certempire.com/vendor/ahima/
- RHIA practice materials: https://certempire.com/exam/rhia-pdf-dumps/
- Update your resume and LinkedIn with measurable wins (turnaround time, audit success, data quality improvements)
Here’s a fast, clean way to act on each item this week.
- Map your target role and location to a realistic range
- Pull 3–5 live postings that match your scope (team size, KPIs, system complexity).
- Log the low/mid/high band for each posting or salary insight you trust.
- Set two numbers: your target base and your stretch ask (with rationale tied to scope).
| Target role + scope | Market/metro | Range to expect (2025) | Source notes | Your target / stretch |
| RHIA generalist, single-campus hospital | Chicago metro | $78k–$95k (mid-to-high band) | Matches national mid-career bands; urban uplift | $90k target / $98k stretch |
| HIM Manager, team of 8–12 | Seattle | $110k–$135k+ | Complex IDN; high cost-of-living market | $125k target / $135k stretch |
| Privacy/Compliance Analyst (healthcare) | Boston area | $85k–$110k | Mid-high due to regulatory scope | $100k target / $108k stretch |
| Data Governance Analyst (vendor, remote) | National band | $90k–$115k (geo-adjust may apply) | Travel and scope can lift comp | $108k target / $118k stretch |
Tip: sanity-check the hourly. Annual ÷ 2080. Example: $100k ≈ $48.10/hr. Helpful in apples-to-apples comparisons.
- Close one skills gap that directly supports scope
Pick one lane. Ship visible impact in 6–8 weeks. Keep it small, real, and tied to KPIs.
| Lane | Mini-project (resume-ready) | Outcome metric | Weekly time |
| Privacy/Security (CHPS track) | Draft and pilot a PHI incident response checklist + 1 tabletop exercise | Time-to-containment cut by 20%; audit-ready artifacts | 3–4 hrs |
| Analytics (SQL/BI basics) | Build a HIM KPI dashboard (ROI turnaround, chart completion) | TAT down 10–15%; weekly trend visibility | 4–5 hrs |
| Data Governance (IG lead) | Define a data dictionary for 15 priority data elements + stewardship roles | Data defect rate reduced; clear ownership | 3 hrs |
What to say in 1:1s: “I’d like to own X metric for the next 6 weeks. Here’s the baseline and the target. OK to proceed?”
- If you’re pursuing RHIA now, line up ethical practice materials and schedule a date
- Lock the exam date first. A real deadline sharpens study.
- Use practice questions with explanations. Track misses by domain, not just score.
- Resources:
- AHIMA vendor resources: https://certempire.com/vendor/ahima/
- RHIA practice materials: https://certempire.com/exam/rhia-pdf-dumps/
| Week | Focus | Deliverable |
| 1 | Baseline mock + domain map | Score report; list top 2 weak domains |
| 2 | Deep dive weak domain #1 | 20 micro-notes; mini-quiz ≥80% |
| 3 | Deep dive weak domain #2 | 20 micro-notes; mini-quiz ≥80% |
| 4 | Full-length timed practice + light review | ≥85% on practice; exam-day checklist |
- Update your resume and LinkedIn with measurable wins
- Use this quick formula: metric + action + system/context + outcome.
- Examples you can adapt:
- Improved ROI turnaround from 5.2 to 3.8 days by redesigning queue rules in Epic; 27% faster processing.
- Led chart completion push across 3 service lines; delinquency down 31% quarter-over-quarter.
- Built HIM KPI dashboard (SQL + Power BI); surfaced coding lag drivers and cut lag by 18%.
- Coordinated HIPAA privacy incident tabletop; reduced response time from 2 hrs to 45 minutes.
- Add your credential line up top: RHIA (active), plus any in-progress credentials with ETA.
Simple cadence to keep momentum
- Calendar 2 blocks/week (45 minutes each) for job market logging and outreach.
- One 30-minute block/week for your skill sprint.
- Monthly: refresh your target and stretch numbers based on new postings and your growing scope.
You’ve got clear levers: scope, skills, and market timing. Move one each week. The comp follows.
FAQs
Is RHIA Salary Higher Than RHIT?
Often, yes. RHIA professionals are more likely to manage enterprise HIM operations, compliance, and data governance, which tend to command higher salaries. RHITs focus more on coding, data integrity, and HIM workflows.
Quick Comparison
| Credential | Typical Scope | Common 2025 Base Band (National) | Role Examples | Notes |
| RHIA | Enterprise HIM ops, data governance, privacy/compliance oversight, leadership | ~$65k–$105k+ (leadership often higher) | HIM Manager, Data Governance Lead, Privacy Manager, Director of HIM | Higher bands in large systems, payers, vendors, and urban/high-cost markets |
| RHIT | Coding/CDI support, HIM workflows, data integrity, registries, ROI | ~$50k–$80k (varies by specialty/market) | HIM Specialist, Coding Analyst, ROI Supervisor, Data Integrity Tech | Strong performers can reach RHIA-adjacent pay in niche or high-demand roles |
Tip: To lift your RHIA ceiling quickly, target larger systems, payer/vendor roles, or privacy/data governance tracks.
Can New RHIA Grads Get Remote Roles?
Sometimes, but hybrid or on-site is more common early on. Remote opportunities tend to open up once you’ve proven independence and delivery.
What helps:
- Show proof of self-management (e.g., capstone or internship results: “Cut ROI turnaround by 15%,” “Completed audit prep tasks on time”).
- Target employers used to distributed teams: payers, health tech vendors, consulting firms, and analytics groups.
- Highlight your home setup: secure workspace, dual monitors, privacy practices, and comfort with collaboration tools.
- Ask for a hybrid ramp: start on-site, move to hybrid, then remote eligibility after performance milestones.
Does a Master’s Degree Help?
For leadership tracks, yes. A Master of Health Administration (MHA) or Master of Health Informatics (MHI) can raise the ceiling and accelerate promotion.
Where it pays off most:
- Manager/Director roles
- Privacy/security leadership
- Enterprise data governance
- Competitive markets (IDNs, academic medical centers, payer/vendor leadership)
Practical tip:
- Use tuition assistance if available—many systems subsidize MHA/MHI programs.
- Pair your degree with measurable wins (policy rollouts, accreditation success, KPI ownership).
- If not ready for a master’s, stack targeted certs and stretch projects—you can still climb without the degree.
Which Add-On Credential Pays Off Fastest?
It depends on your chosen path.
- CHPS (Privacy/Security): Strong ROI if you handle incident response, risk assessments, or HIPAA/HITRUST programs. Often accelerates pay in large systems, payers, and vendors.
- CDIP (Documentation Improvement): Best for revenue integrity and CDI leadership. Valuable where DRG accuracy and denials prevention drive results.
- CHDA (Analytics): Rising quickly. Pairs well with SQL/BI literacy and data governance. Strong in vendor, payer, and IDN analytics teams.
Tip: Don’t just collect letters, align the credential with active job postings in your market. Then take on a project that matches, so you’re paid for the new scope, not just the credential.
How Often Should I Revisit Compensation?
At least annually, with midyear checks when scope expands.
Simple cadence:
- Quarterly: Scan 3–5 fresh job postings that match your scope and geography; note ranges and benefits.
- Midyear: If you’ve added KPIs, taken multi-site oversight, or led an audit/accreditation success, request a market adjustment.
- Annual Review: Bring a one-pager with your metrics, projects, market ranges, and target salary band. Keep it professional, tied to outcomes, and forward-looking.
Bottom line: RHIA salaries generally trend higher than RHIT, especially in governance and leadership tracks. But career trajectory depends less on the credential itself and more on scope, setting, and the measurable outcomes you can deliver.
Make your RHIA prep a little easier.
If you’re ready to take your RHIA (or RHIT) journey to the next level, don’t stop at strategy, equip yourself with the tools that help you deliver. CertEmpire offers a wide range of up-to-date practice exams, detailed answer explanations, and simulated testing environments that mirror real certification experiences.
If you’re preparing for a privacy credential like CHPS, a data analytics exam like CHDA, or expanding into tech-adjacent certifications, CertEmpire gives you resources you can trust. Visit Cert Empire now to explore free demos and curated question banks, and close the gap between your aspirations and your next credential.
Last Updated on by Team CE